Advancing Healthcare Through Good Clinical Practice Standards
The Importance of Good Clinical Practice in Healthcare
Good Clinical Practice (GCP) is a set of internationally recognized ethical and scientific standards that ensure the safety, integrity, and quality of clinical trials involving human participants. GCP guidelines provide a framework for conducting clinical research that protects the rights and well-being of participants while generating reliable data.
Adherence to GCP is crucial in healthcare for several reasons:
Protecting Participants’ Rights and Safety
GCP ensures that individuals who participate in clinical trials are treated ethically and with respect. It requires informed consent, confidentiality, and monitoring of participant safety throughout the study.
Ensuring Data Integrity
By following GCP guidelines, researchers can maintain the accuracy and reliability of data collected during clinical trials. This is essential for drawing valid conclusions about the safety and efficacy of new treatments.
Promoting Research Quality
GCP helps to standardize research practices, leading to higher-quality studies that meet regulatory requirements. This contributes to the credibility of research findings and enhances public trust in healthcare interventions.
Complying with Regulatory Requirements
Many regulatory authorities require adherence to GCP when conducting clinical trials. Compliance with these guidelines is essential for obtaining approval to market new drugs or medical devices.
Facilitating Global Collaboration
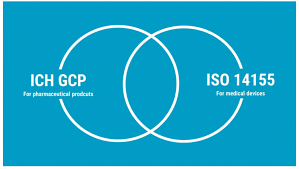
GCP provides a common framework for conducting clinical research worldwide. By following consistent standards, researchers from different countries can collaborate more effectively and share data across international boundaries.
In conclusion, good clinical practice plays a vital role in ensuring the ethical conduct, integrity, and quality of clinical research in healthcare. By upholding these standards, researchers can protect participants, maintain data integrity, promote research quality, comply with regulations, and facilitate global collaboration for the advancement of medical science.
Nine Benefits of Good Clinical Practice: Upholding Ethics, Safety, and Research Integrity
- Ensures ethical treatment of participants
- Protects participants’ rights and safety
- Maintains data integrity and reliability
- Enhances research quality and credibility
- Facilitates compliance with regulatory requirements
- Promotes transparency in clinical trials
- Reduces risks to participants’ well-being
- Encourages global collaboration in research
- Builds public trust in healthcare interventions
Challenges of Good Clinical Practice: Administrative Burden, Costs, Delays, and Complexity for Novice Researchers
- Increased administrative burden
- Higher costs
- Potential delays
- Complexity for inexperienced researchers
Ensures ethical treatment of participants
Ensuring ethical treatment of participants is a fundamental pro of good clinical practice in healthcare. Adhering to ethical standards outlined in GCP guidelines guarantees that individuals involved in clinical trials are treated with dignity, respect, and fairness. This includes obtaining informed consent, maintaining participant confidentiality, and prioritizing their safety and well-being throughout the research process. By upholding these ethical principles, researchers can protect the rights of participants and uphold the integrity of the study, ultimately contributing to the credibility and reliability of research outcomes in the field of healthcare.
Protects participants’ rights and safety
One of the key benefits of adhering to Good Clinical Practice (GCP) guidelines is the protection of participants’ rights and safety during clinical trials. GCP ensures that individuals involved in research studies are treated ethically, with dignity, and respect. By requiring informed consent procedures, confidentiality measures, and ongoing monitoring of participant well-being, GCP safeguards the welfare of those who volunteer to take part in clinical research. This commitment to upholding participants’ rights and safety not only demonstrates ethical conduct but also fosters trust between researchers and study participants, ultimately contributing to the integrity and credibility of the research outcomes.
Maintains data integrity and reliability
Maintaining data integrity and reliability is a crucial benefit of adhering to good clinical practice in healthcare. By following established guidelines and protocols, researchers can ensure that the data collected during clinical trials is accurate, consistent, and trustworthy. This commitment to data integrity not only enhances the credibility of research findings but also enables healthcare professionals to make informed decisions about the safety and efficacy of new treatments. Ultimately, upholding data integrity through good clinical practice contributes to advancing medical knowledge and improving patient care outcomes.
Enhances research quality and credibility
Adhering to Good Clinical Practice (GCP) standards significantly enhances the quality and credibility of research in healthcare. By following rigorous protocols and ethical guidelines, researchers can ensure that their studies are conducted with integrity and produce reliable results. This commitment to high standards not only strengthens the validity of research findings but also boosts confidence in the effectiveness and safety of new treatments or interventions. Ultimately, the emphasis on research quality through GCP promotes transparency, accountability, and trust within the scientific community and among stakeholders, contributing to advancements in medical knowledge and patient care.
Facilitates compliance with regulatory requirements
Facilitating compliance with regulatory requirements is a key advantage of adhering to good clinical practice in healthcare. By following established GCP guidelines, researchers and healthcare professionals can ensure that their clinical trials meet the stringent regulatory standards set by authorities. This not only helps in obtaining necessary approvals for conducting research but also ensures that the data collected is valid and reliable, meeting the criteria needed for regulatory submissions. Ultimately, adherence to good clinical practice streamlines the regulatory process, minimizes delays, and enhances the credibility of research outcomes, contributing to the overall safety and efficacy of healthcare interventions.
Promotes transparency in clinical trials
Promoting transparency in clinical trials is a key benefit of adhering to good clinical practice guidelines. By ensuring that research processes and findings are openly and accurately reported, GCP helps to build trust among stakeholders, including participants, regulators, healthcare professionals, and the public. Transparent clinical trials allow for scrutiny of study methods, data collection, and analysis, ultimately enhancing the credibility and reliability of research outcomes. This transparency also encourages knowledge sharing and collaboration within the scientific community, leading to advancements in medical knowledge and improved patient care practices.
Reduces risks to participants’ well-being
Adhering to Good Clinical Practice (GCP) standards significantly reduces risks to participants’ well-being during clinical trials. By implementing rigorous safety measures, ensuring informed consent, and closely monitoring participants throughout the study, GCP helps protect individuals from potential harm or adverse effects associated with experimental treatments or procedures. This proactive approach not only safeguards the health and safety of participants but also upholds ethical principles and promotes trust in the research process, ultimately contributing to the overall integrity and credibility of clinical research in healthcare.
Encourages global collaboration in research
Good Clinical Practice (GCP) serves as a catalyst for fostering global collaboration in research within the healthcare industry. By adhering to GCP guidelines, researchers from different countries can work together more effectively and efficiently. The standardization of research practices under GCP facilitates the sharing of data and findings across international boundaries, enabling a more comprehensive and diverse approach to addressing healthcare challenges on a global scale. This encourages the exchange of knowledge, expertise, and resources among researchers worldwide, ultimately leading to enhanced collaboration and accelerated progress in medical research and innovation.
Builds public trust in healthcare interventions
Adhering to Good Clinical Practice (GCP) standards significantly contributes to building public trust in healthcare interventions. By following rigorous ethical and scientific guidelines in clinical trials, researchers demonstrate their commitment to ensuring the safety and well-being of participants, as well as the integrity of the data collected. This transparency and accountability not only reassure the public about the reliability of research findings but also enhance confidence in the effectiveness and safety of healthcare interventions developed through these rigorous processes. Ultimately, by upholding GCP principles, healthcare professionals can strengthen trust between patients and the healthcare system, fostering a positive relationship built on integrity and credibility.
Increased administrative burden
Adhering to Good Clinical Practice (GCP) guidelines can present a significant challenge due to the increased administrative burden it imposes. The extensive documentation and reporting requirements mandated by GCP can result in a higher workload for researchers and healthcare professionals involved in clinical trials. This administrative overhead may divert time and resources away from direct patient care and research activities, potentially slowing down the progress of studies and increasing overall costs. Balancing the need for rigorous compliance with GCP standards while managing the administrative workload effectively is crucial to ensure that the benefits of ethical research conduct are not outweighed by the strain on resources and efficiency.
Higher costs
One significant drawback of adhering to Good Clinical Practice (GCP) standards is the potential for higher costs associated with implementing these rigorous guidelines. Meeting GCP requirements often necessitates additional resources, such as specialized training for staff, enhanced monitoring systems, and improved infrastructure to ensure compliance with ethical and regulatory standards. As a result, the financial burden of conducting clinical trials can significantly increase, posing a challenge for research institutions and sponsors seeking to balance the pursuit of high-quality research with cost-effectiveness. The higher costs involved in maintaining GCP standards may limit access to clinical trials for certain populations or hinder the progress of research projects with limited funding resources.
Potential delays
One significant drawback of good clinical practice is the potential for delays in study initiation or completion. The strict adherence to GCP protocols can result in time-consuming compliance activities that may slow down the progress of clinical trials. Researchers and study teams often need to invest additional time and resources to ensure full compliance with the guidelines, which can extend the timeline for starting or finishing a study. These delays can impact the timely availability of new treatments and research outcomes, highlighting a challenge in balancing thorough protocol adherence with efficient study execution.
Complexity for inexperienced researchers
For inexperienced researchers, one significant drawback of good clinical practice is the complexity it presents. Beginners in the field of clinical research may struggle to navigate the intricate requirements of GCP, which can be overwhelming and confusing. The detailed guidelines and procedures set forth by GCP may hinder their ability to conduct studies effectively, as they may require additional training and support to fully understand and implement these standards. This complexity can create barriers for novice researchers, slowing down the research process and potentially impacting the quality and reliability of study outcomes.
